Adoptive cell transfer (ACT) therapy has emerged as a breakthrough approach in cancer treatment. This immunotherapy leverages the power of a patient's own immune system to target and eradicate cancer cells. While chimeric antigen receptor (CAR) T-cell therapy has garnered significant attention, other ACT modalities hold immense promise.
CAR-T Therapy: A Powerful But Limited Approach
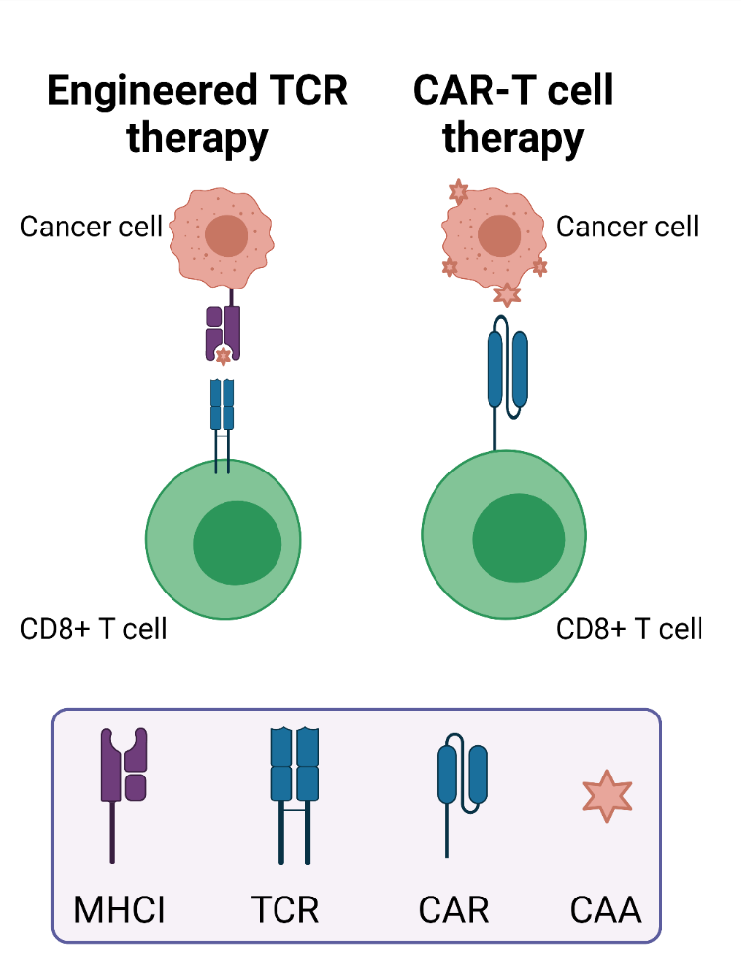
CAR-T therapy involves genetically engineering a patient's T cells to express a novel receptor, the chimeric antigen receptor (CAR). This CAR recognizes a specific antigen on cancer cells, enabling the T cells to identify and eliminate them. CAR-T has demonstrated remarkable success in treating B-cell malignancies, particularly acute lymphoblastic leukemia (ALL) and lymphomas.
However, limitations exist with CAR-T therapy. These include:
- Antigen escape: Tumor cells can lose the targeted antigen, rendering CAR-T cells ineffective.
- Limited efficacy against solid tumors: The tumor microenvironment of solid tumors can hinder CAR-T cell infiltration and function.
- Potential for severe side effects: Cytokine release syndrome (CRS) can be a serious complication.
Maxanim serves as a one-stop shop for researchers in this field, offering all essential reagents.
Expanding the ACT Arsenal: Alternative Strategies
Researchers are actively exploring alternative ACT approaches to overcome these limitations:
1. Tumor-Infiltrating Lymphocytes (TIL) Therapy:
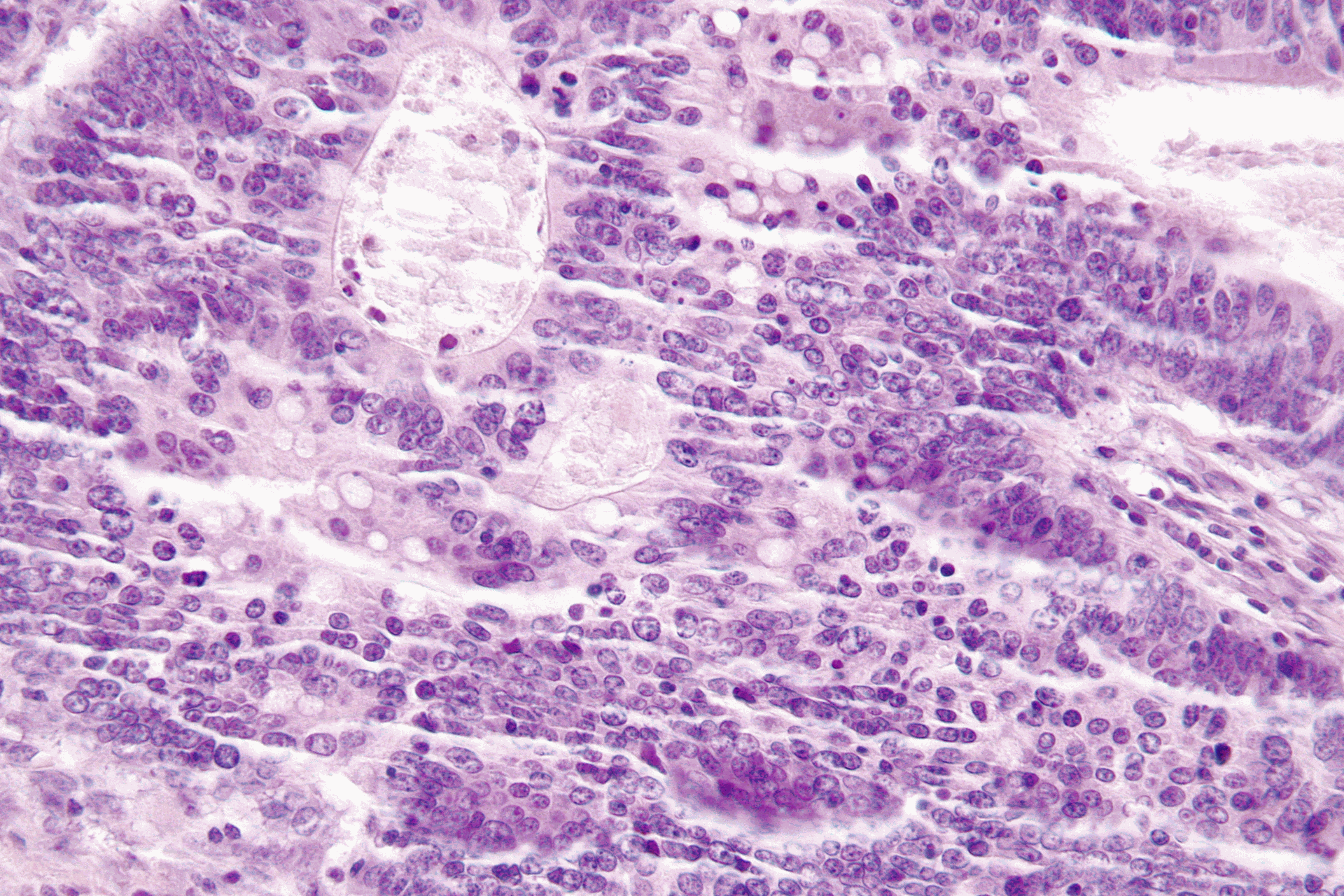
TIL therapy leverages a patient's existing immune response. T cells naturally infiltrate tumors, and TIL therapy isolates these tumor-infiltrating lymphocytes (TILs) from surgically resected tumors. TILs are then expanded in culture and reinfused into the patient to enhance their anti-tumor activity.
TIL therapy shows promise for various solid tumors, including melanoma, and exhibits encouraging clinical results. However, this approach can be time-consuming due to the limited number of TILs often found within tumors.
2. T Cell Receptor (TCR) Therapy:
TCR therapy involves engineering T cells to express a novel T cell receptor (TCR) specific for a tumor-associated antigen (TAA) presented by human leukocyte antigen (HLA) molecules. This approach offers a more targeted strategy compared to CAR-T, potentially reducing off-target toxicities. TCR therapy is currently under clinical investigation for various cancers.
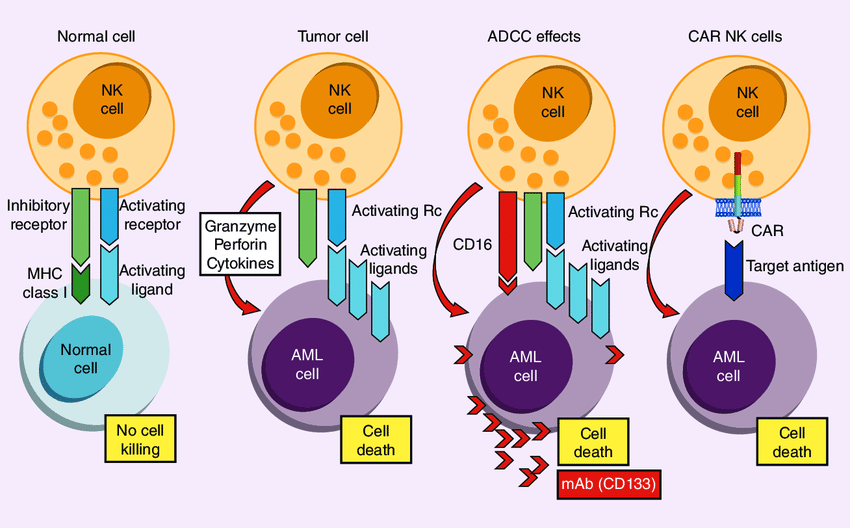
3. Natural Killer (NK) Cell Therapy:
NK cells are innate immune system lymphocytes that can recognize and eliminate tumor cells without prior sensitization. Similar to CAR-T cells, NK cells can be engineered to express CARs, generating CAR-NK cells with enhanced anti-tumor activity. Early clinical trials for CAR-NK therapy are underway, demonstrating promise for the treatment of hematologic malignancies and solid tumors.
The Future of ACT: A Personalized and Multifaceted Approach
The future of ACT lies in a personalized approach, potentially combining different cell types and targeting strategies for optimal efficacy. Researchers are also exploring methods to improve persistence and function of adoptively transferred cells, while mitigating potential side effects.
Conclusion
ACT therapy offers a transformative approach to cancer treatment, with CAR-T therapy leading the charge. However, the field extends beyond CAR-T, with TIL, TCR, and NK cell-based therapies holding immense potential. By harnessing the body's natural defense mechanisms and overcoming current limitations, ACT has the potential to revolutionize cancer treatment across a broad spectrum of malignancies.
Explore CAR T-Cell Therapy in More Detail:
ACT Therapies: Beyond CAR-T for Cancer