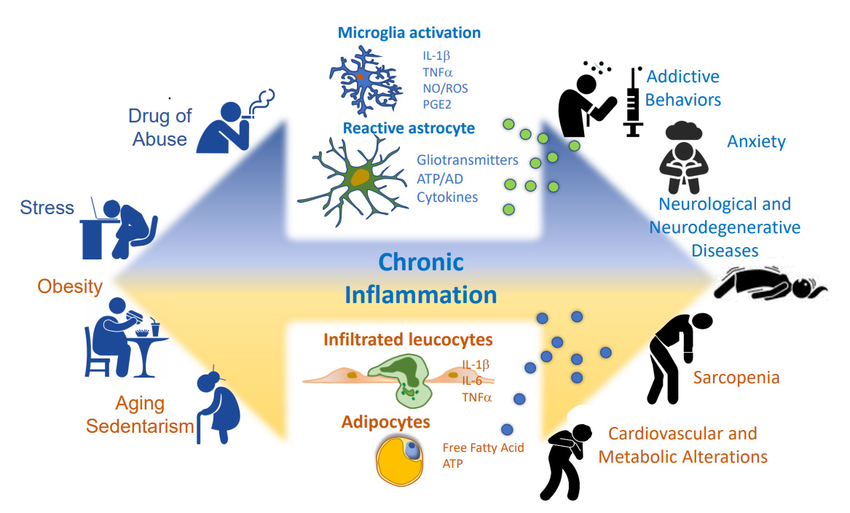
Inflammation is a natural response triggered by the immune system to fight infection or injury. It helps heal tissues and defend against pathogens. However, when this response persists or becomes excessive, it transitions into chronic inflammation, linked to the development of various diseases.
Chronic Inflammation and Disease Development
Acute inflammation is a well-orchestrated process characterized by redness, swelling, heat, and pain. It involves immune cells, chemical messengers (cytokines, chemokines), and the blood vessel system to eliminate the threat and promote healing. But if this response malfunctions or fails to resolve, it becomes chronic inflammation, a persistent low-level immune activation with harmful consequences.
Chronic inflammation is now recognized as a major contributor to many diseases, including:
- Autoimmune diseases: Rheumatoid arthritis, psoriasis, inflammatory bowel disease (IBD).
- Cardiovascular diseases: Atherosclerosis, coronary artery disease.
- Neurodegenerative diseases: Alzheimer's disease, Parkinson's disease.
- Metabolic disorders: Type 2 diabetes, obesity.
- Cancers: Chronic inflammation can promote tumor growth and spread.
Chronic inflammation can damage healthy tissues through prolonged exposure to inflammatory mediators, leading to scarring and organ dysfunction. It can also disrupt cellular balance and promote oxidative stress, both of which contribute to disease progression.
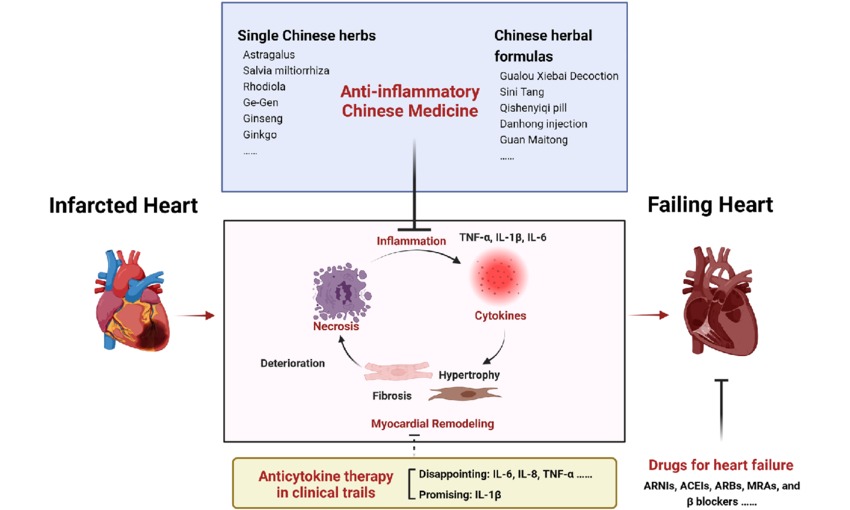
Anti-inflammatory Therapies
Due to the harmful effects of chronic inflammation, developing effective anti-inflammatory treatments is a major focus of medical research. These therapies target different aspects of the inflammatory pathway, offering various treatment options:
- Nonsteroidal anti-inflammatory drugs (NSAIDs): These drugs block enzymes like cyclooxygenase (COX), leading to a decrease in inflammatory prostaglandin production.
- Glucocorticosteroids: Powerful anti-inflammatory and immunosuppressive drugs that suppress the production of pro-inflammatory cytokines.
- Biological agents: Monoclonal antibodies or cytokine receptor antagonists that target specific inflammatory mediators like TNF-α or IL-1β.
The choice of anti-inflammatory therapy depends on the specific disease and the underlying inflammatory pathways involved. Understanding how these therapies work is crucial for optimizing treatment strategies and developing new approaches.
Researchers studying the complex mechanisms of inflammation rely heavily on high-quality research tools. Suppliers like Maxanim offer a wide range of products for this field, including cytokines, antibodies, and ELISA kits. These tools are essential for understanding inflammation and developing new anti-inflammatory therapies.
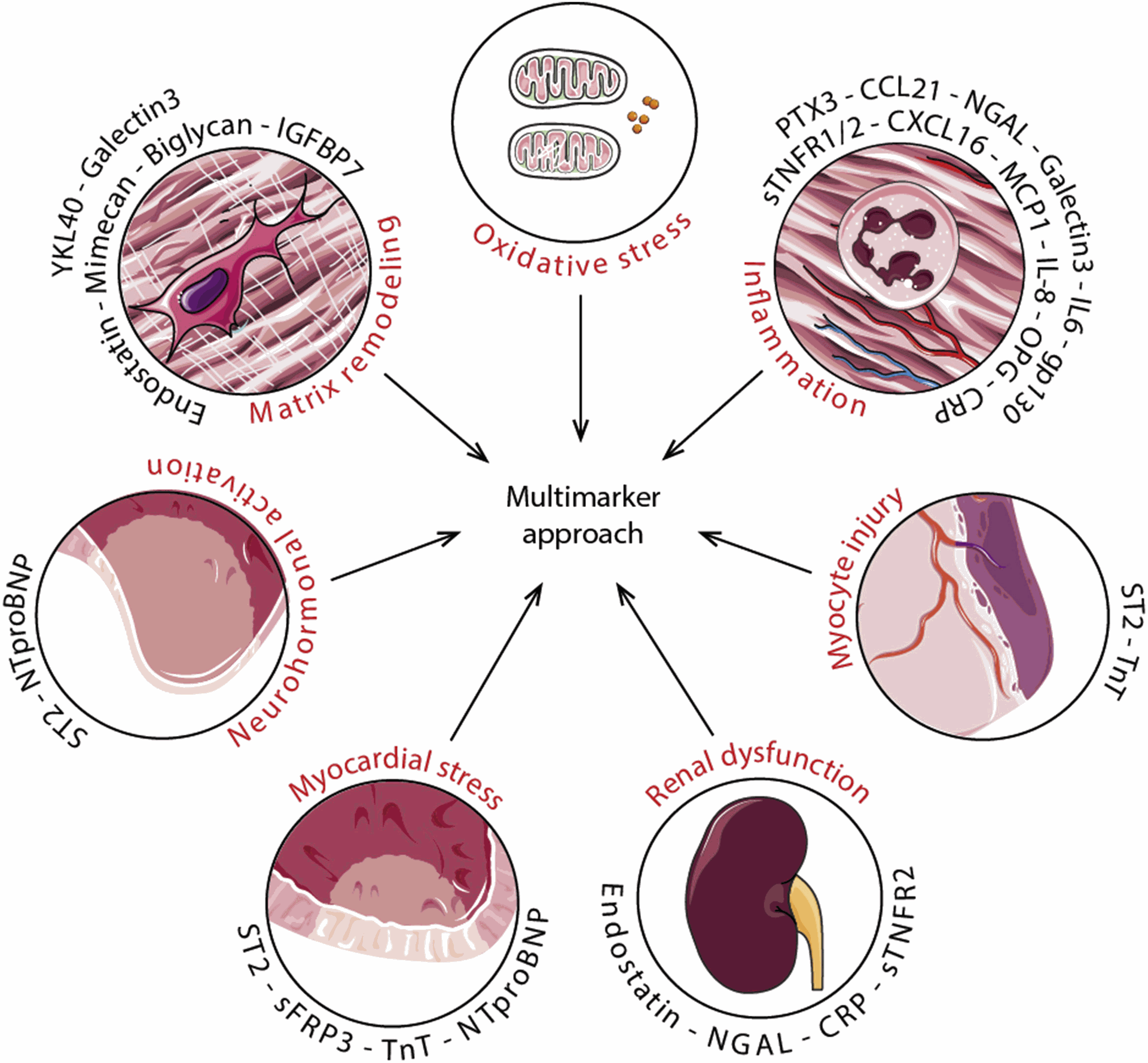
Biomarkers of Inflammation
Biomarkers are measurable biological indicators of a physiological or pathological process. In the context of inflammation, biomarkers offer valuable tools for diagnosing diseases, monitoring disease activity, and assessing treatment response.
Commonly used inflammatory biomarkers include:
- C-reactive protein (CRP): A general marker of inflammation that increases in response to various tissue injuries.
- Erythrocyte sedimentation rate (ESR): Another general marker that indicates the presence of inflammation.
- Cytokines: Specific inflammatory mediators like interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α) can be measured to assess the type and severity of inflammation.
While these biomarkers provide valuable information, the search for more specific and disease-relevant markers is ongoing. Advancements in this field hold significant promise for personalized medicine approaches, allowing for tailored anti-inflammatory therapies based on an individual's unique inflammatory profile.
Conclusion
Chronic inflammation plays a critical role in the development and progression of many diseases. Understanding the mechanisms of inflammation and its contribution to disease paves the way for developing targeted anti-inflammatory therapies and identifying relevant biomarkers. As research in this arena continues, we can expect advancements in diagnostics, personalized treatment strategies, and ultimately, improved patient outcomes.
Inflammation and Disease: A Key Contributor