For many years, people have suspected a link between diet and mental health. Now, research on the gut-brain connection is revealing a surprising amount of interaction between the trillions of microbes living in our intestines and the complex workings of the brain. This blog post explores this new area of science, examining how the gut microbiome can influence brain chemicals, brain function, and even the risk of developing certain brain disorders.
The Gut and Brain: A Two-Way Street
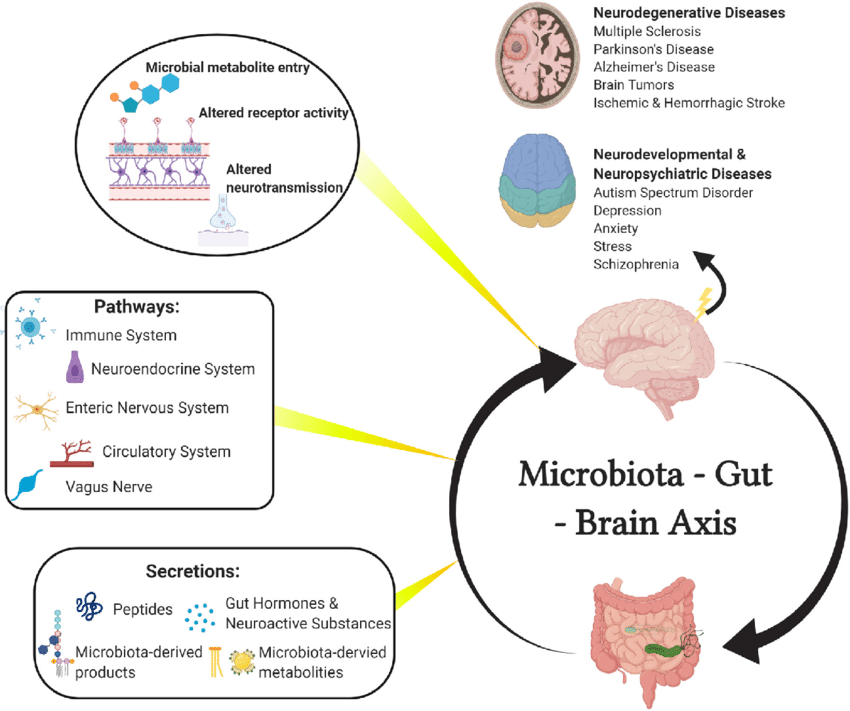
The gut and the brain are in constant communication through a complex pathway called the gut-brain axis. This communication happens in a few ways:
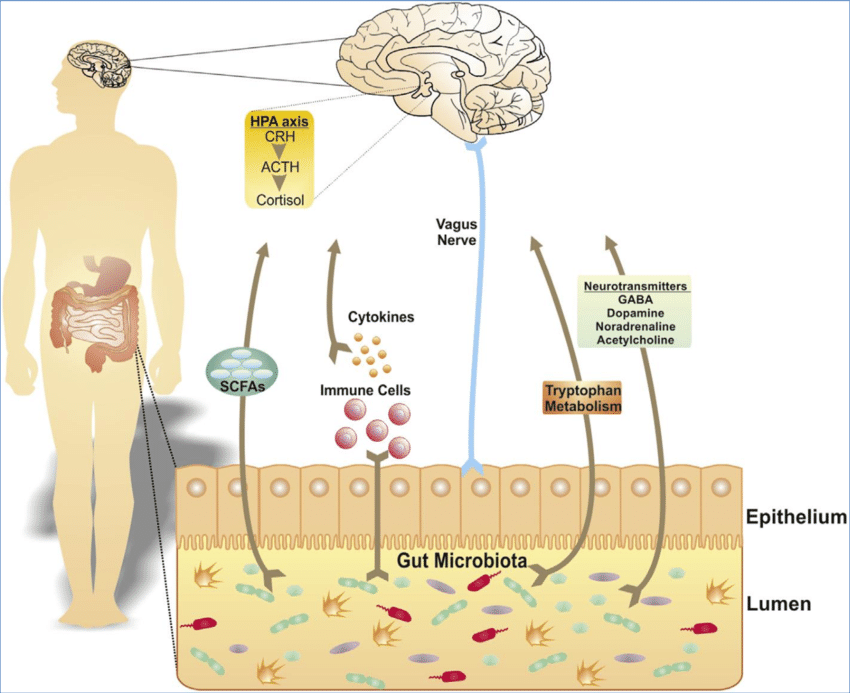
- The Vagus Nerve: This nerve directly connects the gut to the brainstem, sending signals about digestion, inflammation, and nutrient levels.
- The Immune System: Bacteria in the gut can influence the immune system, which can then affect brain function and behavior.
- The Microbiota-Gut-Brain Axis: The gut microbiome, the vast community of microorganisms in our gut, plays a key role in this communication. The gut microbiota produces chemicals that can directly influence brain function and the signaling of brain chemicals.
The Microbiome's Influence on Brain Chemicals
Brain chemicals, called neurotransmitters, play a critical role in mood, thinking, and behavior. Research suggests that the gut microbiome can affect the production, availability, and signaling of important neurotransmitters, including:
- Serotonin: Often called the "happy" chemical, serotonin regulates mood, sleep, and appetite. Studies have shown that certain gut bacteria strains can increase the production of chemicals needed to make serotonin.
- Dopamine: Linked to reward, motivation, and movement, dopamine levels can be impacted by the gut microbiome. Specific bacterial strains have been tied to increased dopamine production in animal studies.
- Gamma-aminobutyric acid (GABA): The main inhibitory neurotransmitter in the brain, GABA promotes relaxation and reduces anxiety. The gut microbiome may influence GABA signaling, potentially affecting mood and stress regulation.
These findings suggest a possible connection between gut dysbiosis (an imbalance in the gut microbiota) and imbalances in brain chemicals, which may contribute to mental health conditions like depression and anxiety.
The Microbiome and Brain Health
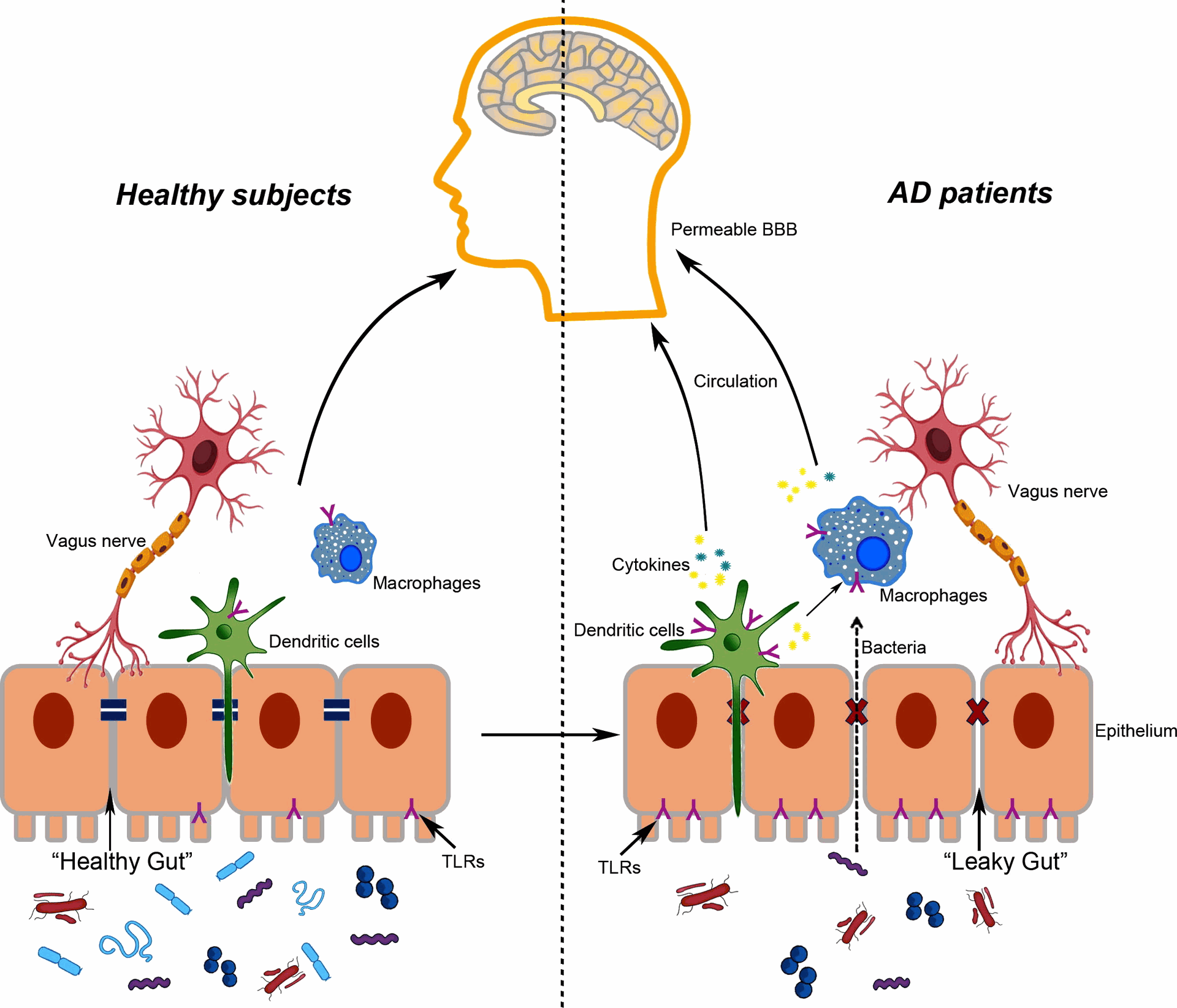
New research is exploring how the gut microbiome might influence the risk and progression of various brain disorders. Studies have found connections between gut dysbiosis and:
- Alzheimer's Disease: Changes in the gut microbiome have been observed in Alzheimer's patients, and some studies suggest that the gut microbiota may play a role in neuroinflammation, a hallmark of the disease.
- Parkinson's Disease: Similar to Alzheimer's, research suggests a possible link between gut dysbiosis and the development of Parkinson's disease, possibly through the influence of the gut microbiome on alpha-synuclein buildup, a key feature of the disease.
- Autism Spectrum Disorder (ASD): Children with ASD often have gut dysbiosis. While the cause-and-effect relationship is unclear, some studies suggest that the gut microbiome may influence brain development processes relevant to ASD.
It is important to note that this is a new area of research, and more investigation is needed to understand exactly how the gut microbiome impacts brain health and the development of brain disorders.
Future Directions: Using the Gut-Brain Connection
The rapidly growing field of gut-brain research holds great promise for developing new treatments for mental health conditions and brain disorders. By understanding how the gut microbiome influences brain function, researchers can explore:
- Prebiotics and Probiotics: These dietary changes may help modify the gut microbiome and potentially improve mental health outcomes.
- Psychobiotics: These are specific strains of bacteria that may offer targeted benefits for mental health conditions.
- Fecal Microbiota Transplantation (FMT): While still under investigation, FMT has shown promise in treating some neurological disorders by restoring a healthy gut microbiome.
The exploration of the gut-brain axis is transforming our understanding of the mind-body connection. The tireless efforts of researchers and the essential support provided by research suppliers such as Gentaur Group are fueling this exciting field. By harnessing the power of the gut microbiome, we may unlock new ways to promote mental well-being and potentially prevent or manage neurological disorders.
The Gut-Brain Connection: How What We Eat Affects How We Think